Optimizing PPE Utilization Based on Inventory Levels
October 30, 2020 | Pharma and Life Sciences 2 minutes read
In recent months, various global and local manufacturers of PPE have increased their production capacities and are operating beyond their normal capacities. Supply additions by PPE manufacturers coupled with government relaxations in PPE regulations have helped increase the supply of PPE to the market. However, the mismatch between supply and demand of PPE items such as masks and respirators makes it important for the companies to draft strategies to optimize the supply of PPE.
Several companies are struggling to find an adequate supply of PPE to ensure the well-being of their workers. Healthcare has witnessed the biggest impact.
PPE Supply Shortage in the Healthcare Sector
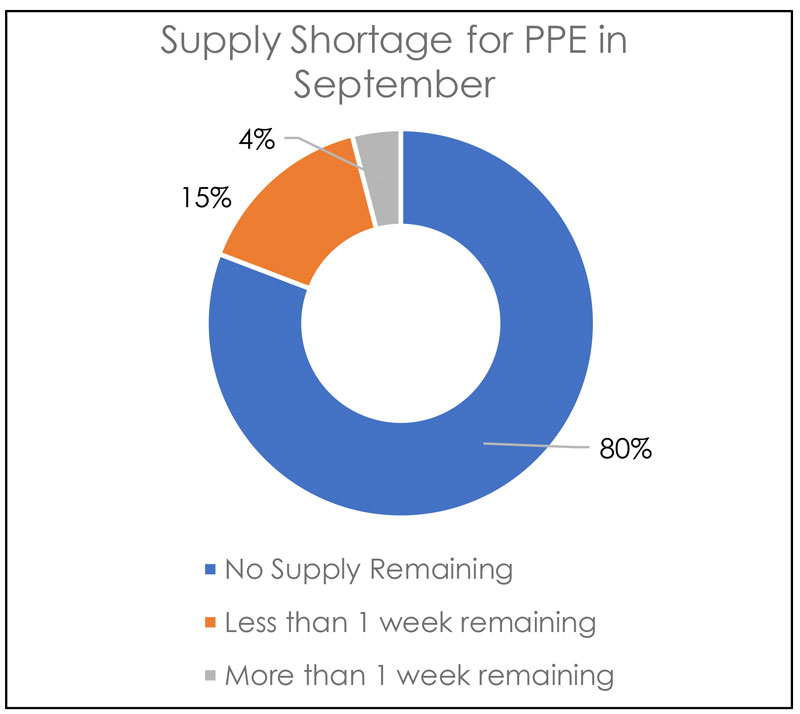
Various healthcare facilities in the US and Europe continue to face PPE shortages as supply chains struggle to build PPE inventories. Large hospital systems have begun to benefit from the recovering supply chains, but smaller facilities are still facing acute PPE shortages. According to Get Us PPE Shortage Index for September, 80% of the companies had no supply for one or more types of PPE. This has led some organizations to clean and sanitize used PPE to extend the life of its existing inventory.
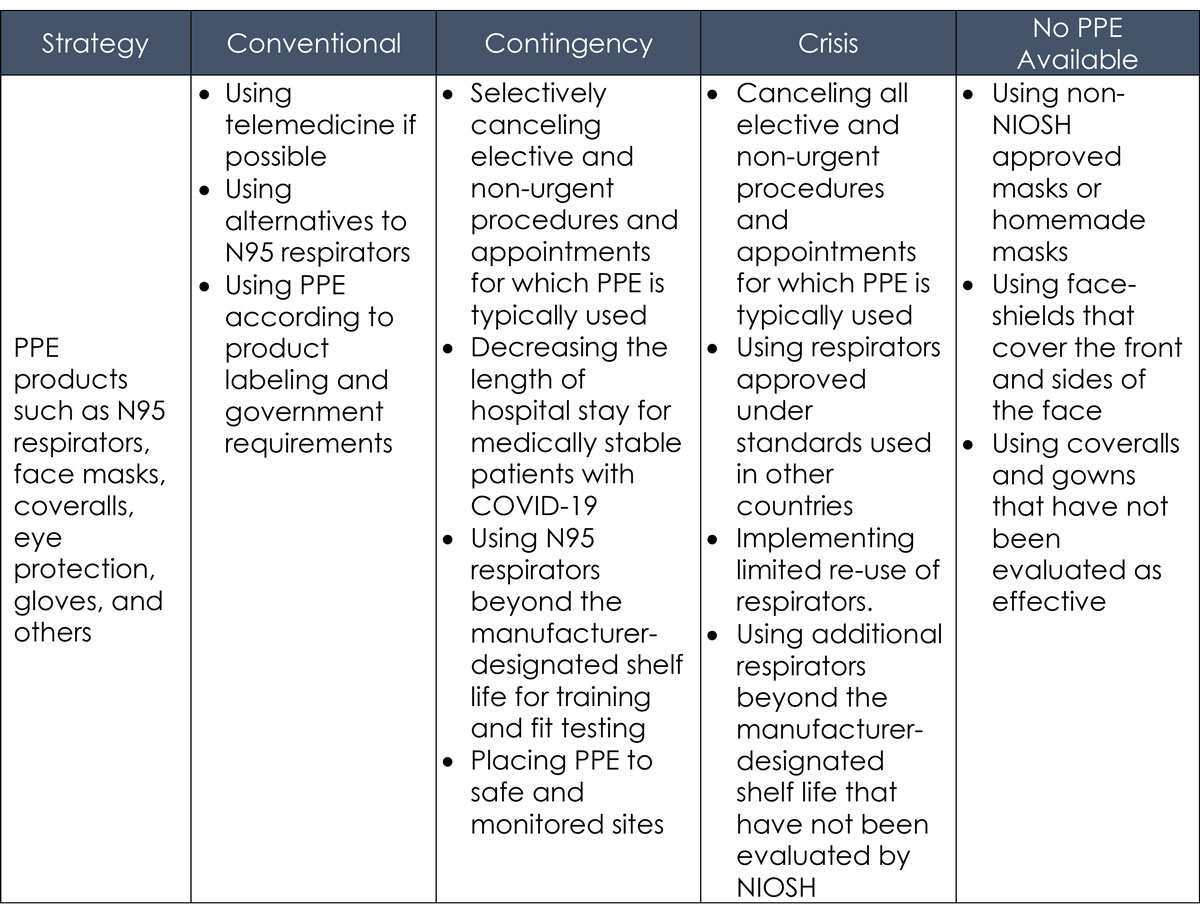
Strategies to optimize the supply of PPE
Organizations must plan to strategically optimize PPE supply to deal with shortages. An interim plan can be implemented as a temporary solution until there is an adequate supply of PPE. The Centers for Disease Control and Prevention (CDC) has developed a Personal Protective Equipment (PPE) Burn Rate Calculator to help facilities plan and optimize the use of PPE for response to COVID-19. Healthcare organizations can leverage the model to describe the *surge capacity into three general strata and use it to prioritize measures to conserve PPE supplies.
Conventional capacity
The capacity consists of PPE that should already be implemented in general infection prevention and control plans in healthcare settings when there are no shortages in PPE supply.
Contingency capacity
The measures that may be used temporarily during periods of anticipated PPE shortages. Contingency strategies can help facilities struggling with supply shortages of PPE, even though it may have a sufficient availability of PPE.
Crisis capacity
Organization should consider crisis capacity strategies when there is not enough supply of PPE to carry out operations or to meet the facility’s current or anticipated utilization.
Strategy Matrix for Healthcare facilities
Best practices while implementing optimization strategies
While implementing these strategies, organizations should consider certain best practices to ensure the optimal utilization of PPE in the organization. Best practices include:
- Proper evaluation of PPE inventories and utilization rate
- Training staff to optimally use PPE
- Implementing the strategies sequentially
- Resuming standard practices as PPE supply returns to normal
*Surge capacity is a measurable representation of the ability to manage a sudden influx of patients.
Sources and References:
- https://getusppe.org/
- https://www.hpnonline.com/regulatory/article/21146439/cdc-updates-on-strategies-to-optimize-supply-of-ppe-and-equipment-during-shortages
- https://www.jointcommission.org/-/media/tjc/documents/covid19/summary-strategies-to-optimize-the-supply-of-ppe-during-shortages-_-cdc.pdf
- https://www.nabh.co/images/COVID19/Strategies%20to%20Optimize%20the%20Supply%20of%20PPE%20and%20Equipment.pdf
- https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/burn-calculator.html
Turn ideas into action. Talk to GEP.
GEP helps enterprise procurement and supply chain teams at hundreds of Fortune 500 and Global 2000 companies rapidly achieve more efficient, more effective operations, with greater reach, improved performance, and increased impact. To learn more about how we can help you, contact us today.

Amol Jawale
Vice President, Consulting
Amol is responsible for leading global teams and building long-lasting strategic client relationships for GEP’s Fortune 500 Pharma & Life Sciences clients.
He has vast experience in leading engagements focused on procurement strategy, delivery management, and competitive assessment and formulating business cases with C-Suite stakeholders to enable sustainable value creation.